This retrospective study aimed to evaluate whether anti-glycoproteins (GPs) autoantibodies can be used as predictors of response to high-dose dexamethasone combined with rituximab (DXM-RTX) in the treatment of primary immune thrombocytopenia (ITP) patients.
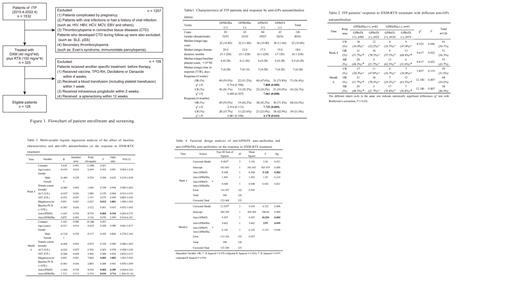
According to the screening criteria (Figure. 1), 126 ITP patients, including 85 (67.5 %) women and 41 (32.5 %) men, were included in the analyses, with a median age was 32 (10 - 80) years, the median duration of disease was 18 (0.1-228.0) months, and the median platelet count at baseline was 6.0 (0-28.0) × 10 9/L.
As shown in Table 1, 56.4% (71/126) of patients responded to DXM-RTX at four weeks, including 43 CR and 28 partial responses. The median time to response (TTR) of 71 responded patients was seven days (range: 4-28 days). The OR rate of ITP patients with anti-GPIb/IX positivity was 47.6% (40/84), while that of anti-GPIb/IX autoantibody-negativity was 73.8% (31/42) (χ 2 = 7.808, P = 0.005). In line with the OR rate, a significant difference was found in the CR rate between ITP patients with anti-GPIb/IX positivity and anti-GPIb/IX autoantibody-negativity (26.2% vs. 50.0%, χ 2 = 7.061, P = 0.008). At six months of DXM-RTX therapy, 54.0% (68/126) of patients responded to DXM-RTX, with 39 (31.0%) of CR. The CR and OR rates of anti-GPIb/IX autoantibody-positive patients were also significantly lower than those of negative patients (CR: 45.2% vs. 71.4%, χ 2 = 7.731, P = 0.005; OR: 25.0% vs. 42.9%, χ 2 = 4.178, P = 0.041). No significant difference ( P > 0.05) was found in OR and CR rates between anti-GPIIb/IIIa autoantibody positive and negative patients at four weeks and six months of DXM-RTX therapy.
At four weeks of DXM-RTX therapy, a significant difference in OR rate was found among the patients with anti-GPIb/IX single-positivity (37.5%), double-positivity (51.7%), double-negativity (68.4%), and anti-GPIIb/IIIa single-positivity (78.3%) (χ 2 = 9.617, P = 0.022) (Table 2). The further comparison revealed a higher resistance to DXM-RTX in patients with anti-GPIb/IX single-positivity than patients with anti-GPIIb/IIIa single-positivity (OR: 37.5% vs. 78.3%; P < 0.05). A similar trend was also found in the six-month OR rate (29.2% vs. 78.3%, P < 0.05). An analysis of the CR rate at four weeks of therapy showed a significant difference among the four groups (χ 2 = 8.523, P = 0.036) but no significant difference after Bonferroni's correction ( P > 0.05). No significant difference ( P = 0.119) was found in the CR rate among the four groups at six months of combined therapy. In addition, the NR rate of patients with anti-GPIb/IX single-positivity also increased significantly in comparison with the patients with anti-GPIIb/IIIa single-positivity at four weeks (62.5% vs.21.7%, P < 0.05) and six months (70.8% vs.21.7%, P < 0.05) of combined therapy.
Multivariate logistic regression analyses revealed that age, sex, duration of disease, liver function, and baseline platelet count were not associated with patient response to DXM-RTX at 4 weeks and 6 months (Table 3). Anti-GPIb/IX autoantibodies and megakaryocytes of DXM-RTX therapy at both 4 weeks and 6 months were associated with the OR rate of patients, with an odds ratio of 0.194 ( P = 0.003, 95% CI: 0.065-0.575) at 4 weeks and 0.189 ( P = 0.003, 95% CI: 0.064-0.563) at 6 months by comparing patients with anti-GPIb/IX autoantibodies to those without anti-GPIb/IX autoantibodies. The factorial design analyses revealed no interaction effect between autoantibodies and showed anti-GPIb/IX autoantibodies at 4 weeks represented the only significant factor affecting OR rate with DXM-RTX therapy (F = 9.128, P = 0.003, Table 4).
Therefore, platelet anti-GPIb/IX autoantibodies can predict poor response to DXM-RTX in ITP patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal